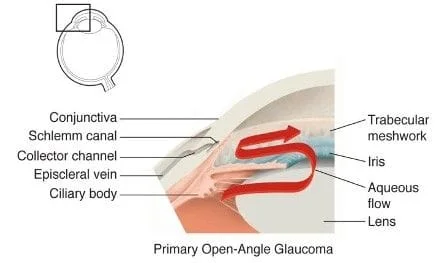
Glaucoma is a leading cause of blindness, both nationally and globally. Along with cataract, glaucoma patients are a large proportion of most ophthalmology practices. Described as the “sneak thief” of sight, glaucoma causes no symptoms. The optic nerve progressively deteriorates due to high intra-ocular pressure, poor circulation, or both. The visual field, both peripheral and central, fades. Eventually blindness can result. Many types of glaucoma exist, but all are defined by glaucomatous optic nerve damage. Like a spinal cord or other nerve injury, a damaged optic nerve cannot be repaired.

Early Primary Open Angles Glaucoma usually has no symptoms at all because the brain combines images from each eye.
Left Eye

Both Eyes

Right Eye

Even in advanced glaucoma the combined vision input from both eyes masks the severity of vision loss.
Left Eye

Both Eyes

Right Eye

Untreated, glaucoma will eventually cause severe visual field loss or complete blindness.

A Glaucoma Suspect shows certain risk factors for glaucoma, such as high intraocular pressure, narrow angles or cupped optic nerves, but does not yet have objectively proven optic nerve damage. When testing shows visual field loss or optic nerve damage we diagnose glaucoma. Ideally we would diagnose glaucoma at an early stage, rather than a more advanced stage.
Glaucoma is not just a disease of high intraocular pressure, but of optic nerve damage that is sensitive to intraocular pressure (IOP). IOP varies from day to day. Many patients have frequently elevated IOP, but no evidence of optic nerve damage. Around one third of glaucoma patients have Normal Tension Glaucoma, also known as Low Tension Glaucoma: no elevated pressure, but glaucomatous optic nerve damage nonetheless. These patients require a careful optic nerve examination for a timely diagnosis. Aside from high intraocular pressure, risk factors for glaucoma include family history of glaucoma, African-American ethnicity, Asian or Native American ethnicity, prior eye trauma or surgery, chronic steroid medication, age over 60, nearsightedness, and certain medical conditions. Often glaucoma runs in the family over multiple generations.
The signs of glaucomatous optic nerve damage are subtle at first. Examination may show thin, pale or asymmetric optic nerves. If examination shows suspicious optic nerves, peripheral vision testing is the next crucial step to catching glaucoma at an early stage. Your brain adeptly fills in blind spots making you unaware of the vision you are losing. At Tennessee River Eye Clinic, we use the Humphrey Visual Field Analyzer to periodically examine your visual fields for damage or progression of prior damage.
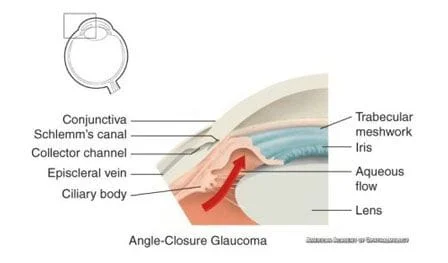
Gonioscopy can detect progressive narrowing of the angle, which may contribute to high IOP. We can also use Heidelberg Engineering Spectralis OCT Anterior Segment Imaging to objectively assess narrowing of the angle. Narrow angle glaucomas are more common in those with hyperopia (far-sightedness), Asian or Native American ethnicity, and over age 60.
Treatment will be based on lowering your intraocular pressure around 20-30% initially, which is called your Target Pressure. If your optic nerve damages progresses, your target pressure is lowered and we continue to watch for further progression. This cycle of treat and observe is repeated until no further progression is seen. The method currently used to measure IOP can be inaccurate for patients with relatively thick or thin corneas. At Tennessee River Eye Clinic we can measure corneal thickness using Sonogauge Corneal Pachymetry and adjust your target IOP for this variable. Frequent IOP checks are done to monitor the effectiveness of treatment. Like diabetics control their blood sugar to prevent complications, glaucoma patients control IOP to prevent optic nerve damage.
Treatment may start with daily eye drops, but as treatment is usually lifelong this decision is significant.


Laser Peripheral Iridotomy, or PI, is done first in narrow angle types of glaucoma to lower IOP or to prevent an attack of potentially devastating Angle Closure Glaucoma.

Cataract Surgery is effective in treating Narrow Angle Glaucoma, and is sometimes needed to open the angle, even if a peripheral iridectomy has been performed. Open Angle Glaucoma patients usually enjoy improved intraocular pressure after routine cataract surgery. Studies confirm that, on average, glaucoma patients require less medications after cataract surgery.
Minimally Invasive Glaucoma Surgery (MIGS) inludes several available and in development implant based procedures designed to surgically treat glaucoma at the time of cataract surgery. Cataract surgery is generally considered to be safe and effective. The goal of all MIGS procedures is to surgically control treat glaucoma while undergoing a very common cataract surgery, with minimal additional risk or recuperation time.
Dr. Kassels has all of these tools available for the optimal management of glaucoma. Dr. Kassels can prescribe eye drops to control IOP. He has Argon laser for ALT, YAG laser for Peripheral Iridotomy, and Lumenis Selecta II SLT laser treatment. He can perform filtration surgery, also known as Trabeculectomy alone or in combination with cataract surgery. Often a combination of therapy is required. Occasionally, these measures are inadequate and he will refer a patient to a glaucoma sub-specialist for more aggressive surgery.

